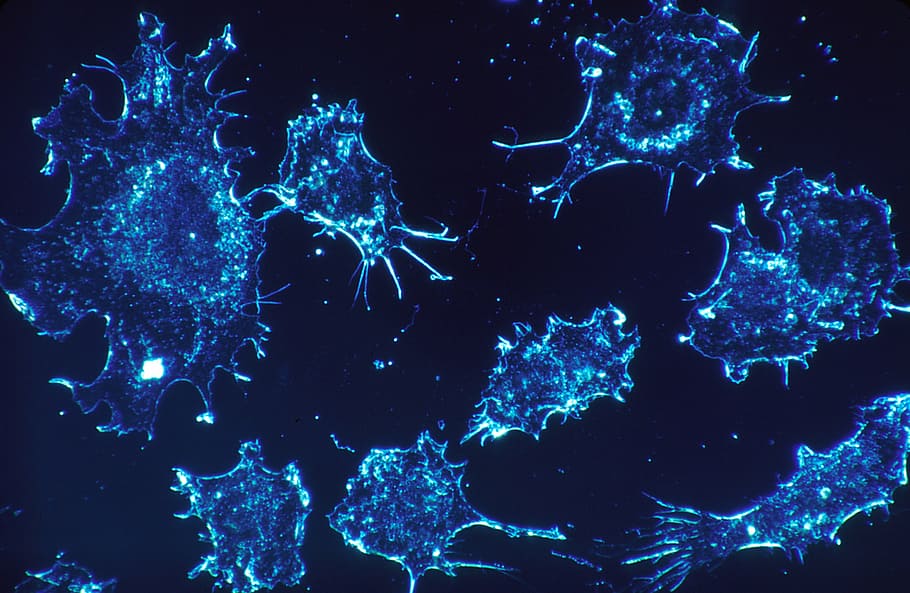
For decades, the dominant paradigm for treating cancer—the uncontrolled growth of abnormal cells—was characterized by a relentless, often brutal, scorched-earth approach, relying heavily on surgery to physically remove tumors, radiation therapy to obliterate localized malignant cells, and chemotherapy, a systemic poison designed to kill rapidly dividing cells throughout the entire body, leading to devastating side effects and often failing to address metastatic or resistant forms of the disease.
This traditional methodology, while saving countless lives, fundamentally treated cancer as an external invasion or a simple mass to be destroyed, entirely overlooking the complex biological interplay occurring within the patient’s own body, particularly the sophisticated, built-in defense mechanisms that govern the body’s self-protection capabilities.
Scientists and clinicians have long harbored the profound suspicion that the key to achieving long-term remission and even cures did not lie in introducing more powerful external toxins but in unlocking and mobilizing the patient’s own immune system, the most specialized and powerful biological surveillance network ever evolved, which possesses the inherent, yet often suppressed, ability to recognize, target, and eliminate abnormal cells with exquisite specificity.
The challenge was never whether the immune system was capable of fighting cancer, but how to circumvent the clever, evasive mechanisms that tumors develop to essentially hide from or actively paralyze the immune response, convincing the T-cells and natural killer cells that the malignant growth was either normal body tissue or a harmless foreign entity.
This intellectual and technological pursuit—the quest to remove the tumor’s immunological mask and reawaken the body’s defenses—has culminated in the revolutionary field known as Cancer Immunotherapy, marking a definitive and incredibly exciting turning point in oncology where the treatment weapon is no longer a harsh chemical but the patient’s own supercharged biology.
Understanding the Immune System and Cancer’s Evasion
To appreciate immunotherapy, one must first grasp the immune system’s basic function and how cancer manages to slip past this sophisticated surveillance.
A. The Core Components of Immune Surveillance
The body’s defense system is divided into two major, interconnected branches.
Innate Immunity: This is the body’s rapid, non-specific first line of defense, involving cells like macrophages and natural killer (NK) cells that quickly attack anything they identify as foreign or damaged without needing prior exposure.
Adaptive Immunity: This is the highly specific, memory-based response, dominated by T-lymphocytes (T-cells) and B-lymphocytes (B-cells), which learn to recognize specific foreign invaders (antigens) and launch a precise, long-lasting attack.
Cancer Antigens: Tumors often express unique proteins or mutated fragments (neoantigens) on their surface, which should, in theory, be recognized by the T-cells as abnormal and trigger a destructive immune response.
B. Cancer’s Evasion Strategies
Tumors are masters of disguise and defense, using several tricks to avoid immune attack.
Loss of Antigen Presentation: Cancer cells can stop displaying their unique antigens on their surface, making them functionally invisible to patrolling T-cells that require a recognizable target to initiate an attack.
Immunosuppressive Microenvironment: Tumors actively recruit and instruct other cells to create a localized environment rich in immunosuppressive signals and cytokines, effectively acting as an invisibility cloak that paralyzes nearby immune cells.
Checkpoint Signaling: Cancer cells co-opt natural “brake” mechanisms (immune checkpoints) that the body uses to prevent the immune system from overreacting and attacking healthy tissue. By displaying ligands for these brakes, the tumor forces the T-cells to shut down.
C. The Concept of Immunoediting
The relationship between cancer and the immune system is a dynamic, evolutionary process.
Elimination Phase: The immune system initially successfully detects and destroys newly arising cancer cells, often before the tumor becomes clinically detectable.
Equilibrium Phase: The immune system and the tumor reach a truce or balance, where the immune system contains the growth but cannot eliminate it, leading to a long, dormant period where the tumor evolves under pressure.
Escape Phase: The tumor eventually acquires mutations and evasion strategies that allow it to overcome immune detection and proliferate uncontrollably, leading to clinically recognizable cancer and metastasis. Immunotherapy aims to reverse this final phase.
Milestone 1 – Checkpoint Inhibitors (The Game Changer)
The discovery and successful clinical use of checkpoint inhibitors is widely considered the biggest breakthrough in modern oncology, transforming the treatment of multiple cancer types.
A. How Checkpoint Blockade Works
This approach focuses on releasing the “brakes” that tumors place on the immune system.
Targeting the PD-1/PD-L1 Pathway: The most successful inhibitors target the PD-1 receptor on the T-cell and/or its partner, PD-L1, often expressed by the tumor cell. When PD-1 binds to PD-L1, the T-cell is told to shut down.
The Unlocking Mechanism: Checkpoint inhibitors (monoclonal antibodies) act as blockers, preventing the PD-1/PD-L1 handshake. This action removes the tumor’s “stop signal,” re-energizing the T-cell and allowing it to launch its destructive attack.
Broad Spectrum Efficacy: These drugs have demonstrated remarkable, long-lasting efficacy in previously hard-to-treat cancers, including melanoma, non-small cell lung cancer, kidney cancer, and Hodgkin lymphoma, achieving durable remissions previously thought impossible.
B. Targeting the CTLA-4 Pathway
The second major checkpoint target that was discovered and developed.
Mechanism of CTLA-4: CTLA-4 is another inhibitory molecule expressed on T-cells, acting as an initial brake on the immune response, particularly in the lymph nodes where T-cells are first activated.
Initial Success in Melanoma: The first approved checkpoint inhibitor, Ipilimumab (anti-CTLA-4), showed significant success in extending the survival of patients with metastatic melanoma, proving the checkpoint concept was viable.
Combination Therapy: Combining anti-CTLA-4 and anti-PD-1/PD-L1 therapies often yields synergistic effects, resulting in higher response rates in some cancer types, although this combination also carries a higher risk of immune-related side effects.
C. Immune-Related Adverse Events (irAEs)
Checkpoint inhibitors carry a unique set of side effects that reflect their mechanism of action.
Autoimmunity Risk: Since these drugs unleash the T-cells, the immune system can occasionally mistakenly attack healthy organs (like the colon, thyroid, liver, or skin), leading to colitis, hepatitis, or endocrinopathies.
Management Protocols: Oncologists must be trained to recognize and manage these irAEs, which typically involve immunosuppressive drugs (like corticosteroids) to dampen the overactive immune response, demonstrating the delicate balance required in this therapy.
Long-Term Durability: Despite the adverse events, the anti-cancer effect often persists long after the drug is stopped, suggesting a durable immune memory against the tumor has been established, which is the hallmark of a true cure.
Milestone 2 – CAR T-Cell Therapy (Living Drugs)
CAR T-Cell therapy represents a revolutionary leap forward, moving beyond drugs to genetically engineering a patient’s own immune cells into “living drugs.”
A. The Process of CAR T-Cell Creation
This therapy is complex, highly personalized, and logistically challenging, involving several detailed steps.
Apheresis and Collection: First, T-cells are collected from the patient’s blood in a process called apheresis, similar to blood donation, separating the white blood cells needed for treatment.
Genetic Reprogramming: The collected T-cells are then sent to a specialized lab where they are genetically modified using a viral vector to express a Chimeric Antigen Receptor (CAR) on their surface.
Expansion and Infusion: These newly engineered CAR T-cells are grown into millions of copies (expanded) and then infused back into the patient, where they are now programmed to hunt down and kill cancer cells expressing a specific target antigen.
B. Success in Hematological Malignancies
CAR T-Cell therapy has achieved its most dramatic results in certain blood cancers.
Acute Lymphoblastic Leukemia (ALL): CAR T-cells targeting the CD19 antigen found on B-cells have achieved remarkable cure rates (often over 80%) in children and young adults with relapsed or refractory B-cell ALL, where no other treatment options remained.
B-Cell Lymphomas: Similar success has been found in refractory Diffuse Large B-Cell Lymphoma (DLBCL) and other B-cell lymphomas, often leading to complete and long-lasting remission after a single infusion.
Current Limitations: While incredibly potent, CAR T-cell therapy is currently approved only for blood cancers, as designing CAR T-cells that safely and effectively penetrate and attack solid tumors remains a significant challenge.
C. Unique Toxicities and Management
CAR T-Cell therapy comes with specific, acute side effects requiring specialized hospital care.
Cytokine Release Syndrome (CRS): This is a potentially life-threatening systemic inflammatory response that occurs when the massively activated CAR T-cells release high levels of inflammatory molecules (cytokines), causing high fever, low blood pressure, and organ dysfunction.
Neurotoxicity (ICANS): Some patients experience Immune Effector Cell-Associated Neurotoxicity Syndrome (ICANS), leading to confusion, seizures, and difficulty speaking, requiring intensive monitoring and specific counter-therapies.
Role of Tocilizumab: The severity of CRS can often be managed effectively using Tocilizumab, a monoclonal antibody that blocks the receptor for Interleukin-6 (IL-6), a key cytokine driving the syndrome, demonstrating the rapid advancement in supportive care.
Milestone 3 – Oncolytic Viruses and Vaccines
![]()
These two modalities represent ways to either directly kill cancer cells or provide the immune system with the necessary training data to attack the tumor.
A. Oncolytic Virus Therapy
Using genetically engineered viruses to selectively destroy cancer cells and stimulate an immune response.
Mechanism of Action: The viruses are genetically modified to replicate selectively within cancer cells (leaving healthy cells untouched), causing the cancer cell to burst (lysis). This lysis releases tumor-specific antigens and danger signals.
Dual Role: The virus acts as a two-in-one punch: it directly kills tumor cells physically, and the resulting release of antigens trains and activates the patient’s own T-cells to recognize and attack any remaining, untreated cancer cells.
Combination Power: Oncolytic viruses have shown promise in synergy with checkpoint inhibitors, acting as a localized immune primer that turns immunologically “cold” tumors (those ignored by the immune system) into “hot” tumors ready for checkpoint blockade.
B. Therapeutic Cancer Vaccines
Teaching the patient’s immune system to recognize specific tumor targets before or after diagnosis.
Focus on Personalized Vaccines: Unlike preventative vaccines (like HPV), therapeutic cancer vaccines are often highly personalized. Tumor tissue is sequenced to identify unique neoantigens, and a vaccine is custom-made to expose the patient’s immune system to those specific targets.
Dendritic Cell Vaccines: One notable approach involves collecting the patient’s own dendritic cells (the immune system’s master presenters), loading them with tumor antigens in a lab, and re-infusing them to efficiently train T-cells in vivo.
Future Integration: While initial vaccine trials had limited success alone, they are now being re-evaluated for use in combination with checkpoint inhibitors, where the vaccine provides the target information and the inhibitor provides the necessary release of the brakes.
C. Adoptive Cell Transfer (ACT)
A foundational technique focused on isolating and expanding tumor-specific T-cells.
Tumor-Infiltrating Lymphocytes (TILs): T-cells that have already found their way into the tumor are isolated from the surgically removed tissue. These Tumor-Infiltrating Lymphocytes (TILs) are known to be cancer-specific.
Massive Expansion: The TILs are grown in the lab into billions of cells (a 1,000-fold expansion) and then infused back into the patient, giving the immune system an overwhelming, targeted strike force against the cancer.
Efficacy in Solid Tumors: ACT using TILs has shown particular promise in metastatic melanoma and cervical cancer, offering a powerful method to deliver highly specific anti-tumor immunity directly into solid tumor microenvironments.
The Future Landscape and Unsolved Challenges
Despite the incredible progress, immunotherapy faces hurdles related to cost, resistance, and efficacy in specific cancer types.
A. The Challenge of Non-Responders
A significant number of patients, particularly those with common solid tumors, still do not respond to existing immunotherapies.
Immunologically “Cold” Tumors: Many common cancers (e.g., prostate, pancreatic, glioblastoma) are poorly infiltrated by T-cells and do not express enough PD-L1, making them inherently resistant to current checkpoint inhibitors.
Mechanisms of Primary Resistance: Researchers are intensely studying why some tumors never respond (primary resistance), which may involve other, as-yet-undiscovered checkpoint pathways, or structural barriers that physically block immune cell entry.
Acquired Resistance: Tumors that initially respond may later evolve to become resistant (acquired resistance), often by losing the target antigen or switching on alternative immune evasion pathways, necessitating continuous monitoring and adaptive treatment strategies.
B. Affordability and Access
The revolutionary nature of these therapies comes with an immense financial cost.
High Price Tag: Immunotherapies, particularly CAR T-Cell therapy and checkpoint inhibitors, are among the most expensive drugs in history, with costs often exceeding hundreds of thousands of dollars per patient, raising major questions about global equitable access.
Manufacturing and Logistics: CAR T-Cell therapy is a highly complex, personalized process that requires sophisticated, centralized manufacturing facilities and a flawless “vein-to-vein” logistical chain, limiting its availability globally.
Need for Biomarkers: A major focus is identifying reliable predictive biomarkers (e.g., Tumor Mutational Burden, PD-L1 expression levels) to determine which patients are most likely to respond before committing them and the healthcare system to the massive cost and risk of treatment.
C. Next-Generation Immunotherapy Strategies
The field is aggressively moving toward novel combinations and targeting new molecules.
Targeting Alternative Checkpoints: New research is focused on blocking lesser-known inhibitory pathways (e.g., LAG-3, TIGIT, TIM-3) either alone or in triple combination with PD-1 and CTLA-4 to overcome resistance.
Bi- and Tri-Specific Antibodies: Developing antibodies that can simultaneously bind to two or three different targets—for instance, one to the tumor, one to the T-cell—to physically bring the immune cell and the cancer cell into close proximity for a guaranteed attack.
Universal CAR T-Cells (Off-the-Shelf): Research is underway to create allogeneic (donor-derived) CAR T-cells that can be manufactured in large batches and stored, making the therapy instantly available, less expensive, and scalable, resolving the major logistical bottleneck of personalized therapy.
Conclusion
![]()
Immunotherapy has fundamentally redefined cancer treatment, moving beyond crude destruction toward sophisticated biological warfare orchestrated by the patient’s own cells.
The discovery of checkpoint inhibitors, particularly the PD-1/PD-L1 pathway, was the monumental breakthrough that first allowed scientists to remove the tumor’s immunological brakes and unleash the T-cells.
CAR T-Cell therapy represents the cutting edge, turning a patient’s immune cells into genetically engineered, highly potent “living drugs” with curative power against previously incurable blood cancers.
Techniques such as therapeutic cancer vaccines and oncolytic viruses are actively being refined to serve as crucial primers, teaching the immune system precisely what the cancer targets look like.
Despite the incredible successes, the field is heavily focused on overcoming the significant challenge of treating patients with immunologically “cold” solid tumors that remain resistant to current therapies.
Key future developments involve the strategic targeting of alternative checkpoint pathways and the creation of standardized, “off-the-shelf” universal CAR T-cells to improve global accessibility and reduce staggering costs.
Ultimately, the future of oncology lies in mastering the body’s innate defenses, transforming cancer from an immediate death sentence into a manageable chronic condition, or even a curable disease through the power of personalized immunity.