For more than half a century, the organ transplant waiting list has been one of modern medicine’s most tragic and enduring symbols. It is a silent, agonizing lottery, where hundreds of thousands of people worldwide wait in hope for a pager to buzz, for a phone call in the dead of night that signifies a second chance at life. For far too many—as many as 20 people every single day in the United States alone—that call never comes. The gap between the number of organs available and the number of people who need them is a vast, unbridgeable chasm.
This grim reality, however, is finally on the precipice of a monumental change. We are living at the dawn of a new era, one where “donor” may no longer mean a human tragedy but rather a laboratory procedure. The field of regenerative medicine, a domain once relegated to science fiction, is moving with astonishing speed from the theoretical to the clinical. As of 2025, the promise of lab-grown, bioengineered organs is no longer a question of “if,” but “when.”
This technological revolution promises to do more than just shorten the transplant list; it promises to eliminate it entirely. It promises a future where a patient needing a kidney, liver, or heart can have one custom-built from their own cells, eradicating the lifelong threat of organ rejection and the prison of immunosuppressant drugs. This article will explore the groundbreaking technologies making this future possible, the incredible successes already achieved, the immense hurdles that remain, and the profound impact this will have on human health and longevity.
The Tyranny of the Waiting List
To understand the magnitude of the coming revolution, we must first grasp the severity of the crisis it aims to solve. The current transplant system, for all its life-saving successes, is fundamentally broken by a single, inescapable fact: scarcity.
The demand for organs—kidneys, livers, hearts, lungs, and pancreases—dramatically outstrips the supply from both deceased (cadaveric) and living donors. This chronic shortage creates a brutal system of triage, where patients are prioritized by sickness level, blood type, and time spent waiting.
Even for the fortunate few who receive a transplant, the ordeal is far from over. The new organ, sourced from another person, is immediately identified by the recipient’s body as a “foreign invader.” This triggers a powerful immune response, a lifelong battle called organ rejection. To prevent this, transplant recipients must take a powerful cocktail of immunosuppressant drugs for the rest of their lives. These drugs, while life-saving, are a blunt instrument. By weakening the entire immune system, they leave patients vulnerable to infections, cancers, and severe side effects like kidney damage (ironically) and diabetes. It is, in effect, trading one disease for another.
It is this dual crisis—scarcity and rejection—that bioengineering seeks to conquer.
The Architects of Life: How to Build an Organ

Creating a complex, functional human organ from scratch is arguably the single greatest challenge in modern biology. It requires replicating the work of millions of years of evolution. As of 2025, scientists are attacking this problem from several ingenious angles, with two methods showing the most promise: decellularization and 3D bioprinting.
A. The “Ghost Organ” Method (Decellularization and Recellularization) This is one of the most mature and visually stunning techniques in regenerative medicine. The process works by taking an organ from a donor—often a pig, due to their similar organ size—and “washing” it.
- Decellularization: The organ is perfused with a special solution of enzymes and detergents. This process gently strips away all the original donor cells, DNA, and cellular material.
- The Scaffold: What remains is a perfect, pearlescent-white “ghost organ.” This is the organ’s natural extracellular matrix, or scaffold—the intricate 3D structure of proteins (like collagen and elastin) that gives the organ its shape, architecture, and, most importantly, its complex network of blood vessels.
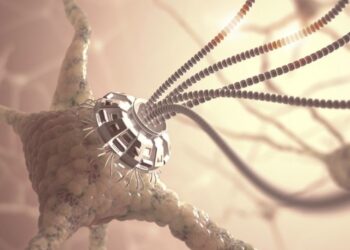
- Recellularization: This is where the magic happens. Scientists take a small biopsy of the patient’s own cells (e.g., skin or blood cells) and, using iPSC technology (more on this later), convert them into the specific stem cells needed for that organ (like kidney cells or liver cells).
- Seeding the Organ: These new, patient-derived cells are injected into the ghost scaffold. The cells naturally recognize the structure and begin to multiply, spreading throughout the scaffold and repopulating it, effectively “bringing it back to life.”
- The Bioreactor: The repopulating organ is placed inside a “bioreactor,” a sophisticated device that acts as an artificial body. The bioreactor pumps warm, oxygen-rich blood, nutrients, and growth factors through the organ, simulating the body’s environment and encouraging the cells to mature into a functional, living tissue.
The primary benefit of this method is that it solves the vascularization problem; the “plumbing” of the organ is already perfectly preserved.
B. 3D Bioprinting: Building from the Ground Up If the scaffold method is like renovating an old house, 3D bioprinting is like building a new one from the blueprint up. This technology has evolved dramatically from printing simple plastics to printing living, biological structures.
- The Blueprint: The process begins with a detailed 3D scan (an MRI or CT scan) of the patient’s own organ, creating a precise digital blueprint.
- The “Bio-Ink”: The “ink” used by the printer is a high-tech hydrogel, a biocompatible substance that is loaded with millions of the patient’s own stem cells. Different types of cells (e.g., muscle cells, vascular cells) can be loaded into different print heads.
- The Printing Process: The 3D bioprinter meticulously deposits the bio-ink layer by tiny layer, following the digital blueprint. It can precisely place different cell types exactly where they need to be, building a complex structure from nothing.
- Maturation: After printing, the structure is placed in a bioreactor, much like the scaffold-grown organ, to allow the cells to mature, fuse together, and begin functioning as a cohesive tissue.
While simpler tissues like skin, cartilage, and even blood vessels have been successfully printed and implanted, the primary challenge for 3D bioprinting remains vascularization. Printing the massive, intricate network of capillaries and blood vessels required by a solid organ like a liver is incredibly complex. However, breakthroughs in printing “vascular trees” and “sacrificial inks” (which print hollow channels that are later flushed out) are bringing this goal closer to reality every day.
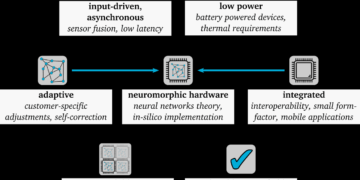
C. The Master Key: iPSCs (Induced Pluripotent Stem Cells) Both of these methods are powered by one of the 21st century’s greatest discoveries: induced pluripotent stem cells (iPSCs).
In 2006, scientist Shinya Yamanaka discovered how to take a mature, specialized adult cell (like a skin cell) and “reprogram” it, winding back its developmental clock to turn it into an embryonic-like stem cell. These iPSCs are “pluripotent,” meaning they have the potential to become any other cell type in the human body.
This technology is the linchpin of personalized regenerative medicine. It means doctors can create an infinite supply of stem cells from a patient, differentiate them into heart, kidney, or liver cells, and then use those cells to build a new organ. Because this new organ is built from the patient’s own genetic material, the body recognizes it as “self.” This is the ultimate goal: a 100% rejection-proof organ, completely eliminating the need for lifelong immunosuppressant drugs.
The Bridge to the Future: Xenotransplantation

While the world waits for fully bioengineered organs to become routine, another, parallel field has surged ahead in the early 2020s, providing a vital “bridge” solution: xenotransplantation.
Xenotransplantation is the process of transplanting an organ from one species to another, and the source animal of choice is the pig. Pig organs are remarkably similar in size and function to human organs. The historical barrier has always been hyperacute rejection—the human immune system violently attacks pig tissue within minutes.
The advent of CRISPR gene-editing has changed everything.
- In landmark procedures in 2023 and 2024, surgical teams successfully transplanted pig hearts and kidneys into human patients.
- These were not just any pig organs. They were “humanized” organs from pigs that had undergone multiple genetic edits.
- Scientists “knocked out” pig genes responsible for triggering human immune rejection and “knocked in” human genes that help the human body accept the organ.
While these patients still require immunosuppression, xenotransplantation proves that a non-human organ source is viable. This technology is seen as a critical stopgap, potentially supplying organs to the thousands of patients who would otherwise die waiting for the fully personalized, lab-grown organs of the next generation.
The Immense Hurdles on the Flight Path
The journey from a laboratory marvel to a routine surgical procedure is long and fraught with immense scientific, financial, and regulatory challenges.
A. The Vascular and Functional Challenge: As mentioned, creating the microscopic network of capillaries that deliver oxygen to every cell in a dense organ is the field’s greatest technical barrier. A secondary, equally difficult challenge is functionality. It is one thing to build an object with the shape of a kidney; it is another entirely to build one that impeccably filters blood, manages blood pressure, and responds to the body’s complex hormonal signals.
B. The Regulatory and Financial Gauntlet: This technology represents a completely new class of medicine. Regulatory bodies like the U.S. Food and Drug Administration (FDA) have no existing framework for approving a “living, custom-built organ.” The clinical trials required to prove both safety and long-term efficacy will be unimaginably complex and astronomically expensive, costing billions of dollars. This high cost of development means the first “off-the-shelf” organs will likely be incredibly expensive, raising profound ethical questions.
C. The Ethical and Social Labyrinth: Who will get these organs first? Will this technology only be available to the wealthy, creating a new, biological class divide? What are the unforeseen long-term health consequences of implanting a lab-grown organ? As for xenotransplantation, it raises its own set of concerns about animal welfare and the small-but-real risk of cross-species viral transmission.
D. The Manufacturing and Scale-Up Problem: Once the technology is perfected, how do we scale it? We will need to transition from an artisanal, university-lab process to a global, industrial-scale manufacturing pipeline. This will require building “organ foundries”—highly-specialized, sterile facilities that can automate the process of growing, maturing, and testing millions of organs per year.
Conclusion: The End of Waiting is in Sight

Despite these formidable challenges, the momentum is undeniable. We have already entered the era of regenerative medicine. Lab-grown skin is routinely used for burn victims. Lab-grown bladders and tracheas have been successfully implanted in patients. And “organoids”—tiny, functional mini-organs grown in petri dishes—are already revolutionizing pharmaceutical research, allowing for drug testing on human-like liver and lung tissue, ending the need for animal models.
The transplant waiting list, that somber artifact of 20th-century medicine, is now on borrowed time. The question is no longer whether we can build new organs, but how quickly we can perfect them and make them accessible. This revolution promises more than just a cure for organ failure; it promises a fundamental shift in how we treat chronic disease and approach human longevity. The bio-factories of tomorrow are being built in the labs of today, and with them, a future where no one ever has to die waiting for a second chance at life.